The relationship between nutrition and male reproductive anatomy has sparked countless myths and misconceptions, particularly regarding whether specific foods can increase testicle size. This topic generates significant interest among men concerned about their reproductive health, yet much of the information circulating online lacks scientific foundation. Understanding the biological realities of testicular development and the role of nutrition in male reproductive health requires examining both anatomical facts and evidence-based research. While certain nutrients undoubtedly support optimal testicular function and hormone production, the notion that dietary interventions can physically enlarge testicles represents a fundamental misunderstanding of male reproductive biology.
Anatomical structure and normal testicular size parameters
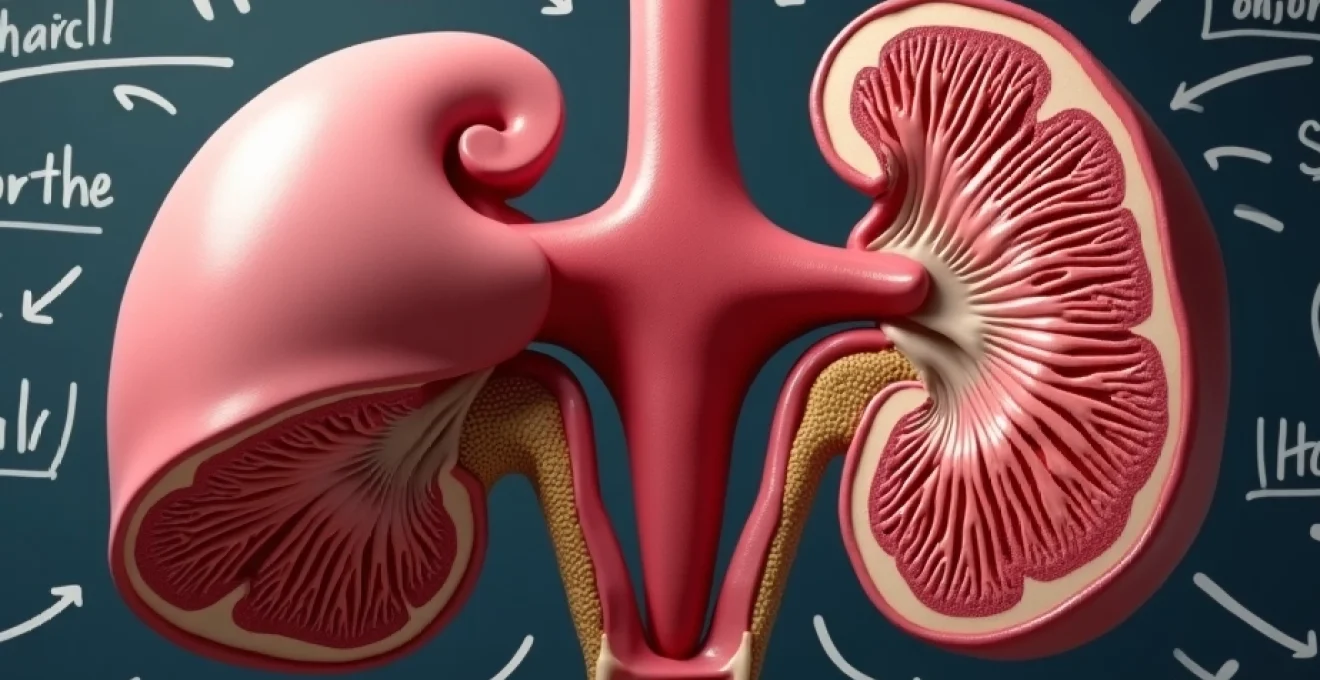
The human testicle represents a complex organ with sophisticated internal architecture designed for dual functionality: hormone production and spermatogenesis. Understanding normal testicular dimensions provides crucial context for evaluating claims about size enhancement through dietary means. Adult testicles typically measure between 4.5 to 5.1 centimeters in length, with volumes ranging from 15 to 25 milliliters. These measurements reflect the intricate balance of various cellular components within the testicular structure.
Testicular volume measurement using prader orchidometer standards
Medical professionals utilise standardised measurement tools, particularly the Prader orchidometer, to assess testicular volume accurately. This beaded chain instrument provides reference points for determining whether testicles fall within normal size parameters. Testicles measuring below 3.5 centimeters in length are considered small, though size variations rarely correlate with functional capacity. The orchidometer measurement system demonstrates that testicular volume exists within established ranges, with genetic factors primarily determining individual variations rather than dietary influences.
Seminiferous tubule development during puberty
The seminiferous tubules, comprising approximately 80% of testicular volume, undergo dramatic changes during puberty under hormonal influence. These microscopic structures house the process of spermatogenesis and expand significantly during adolescent development. However, once puberty concludes, tubular diameter and overall testicular dimensions become relatively fixed. The seminiferous tubules reach their mature configuration by age 18-20 , establishing the permanent structural framework that dietary interventions cannot meaningfully alter.
Leydig cell distribution and interstitial tissue composition
Leydig cells occupy the interstitial spaces between seminiferous tubules and serve as the primary testosterone-producing structures within the testicle. These specialised cells respond to luteinising hormone signals from the pituitary gland, initiating testosterone synthesis. The distribution and number of Leydig cells remain relatively constant throughout adult life, with cellular function rather than quantity determining hormonal output. Nutritional factors may influence Leydig cell efficiency but cannot increase their population or expand testicular volume through cellular proliferation.
Genetic factors influencing testicular dimensions
Hereditary factors exert the strongest influence on testicular size, with family history providing the most reliable predictor of individual testicular dimensions. Genetic variants affecting hormone receptor sensitivity, growth factor expression, and cellular development patterns establish the biological framework for testicular architecture. Environmental factors during foetal development and early puberty may modify genetic expression to some degree, but adult dietary interventions cannot override established genetic programming. Understanding this genetic foundation helps explain why nutritional approaches cannot fundamentally alter testicular size .
Nutritional compounds and androgenic hormone production
While foods cannot increase testicle size, specific nutrients play critical roles in supporting optimal testicular function and hormone production. The relationship between nutrition and male reproductive health operates through biochemical pathways that influence cellular metabolism, hormone synthesis, and protective mechanisms against oxidative damage. These nutritional effects primarily enhance existing testicular capacity rather than expanding physical dimensions.
Zinc deficiency impact on testosterone synthesis pathways
Zinc serves as an essential cofactor in multiple enzymatic reactions involved in testosterone biosynthesis. Deficiency in this mineral can significantly impair Leydig cell function, leading to reduced testosterone production and potentially affecting testicular health. Research demonstrates that men with adequate zinc status maintain more robust hormonal profiles compared to those with deficiencies. However, zinc supplementation cannot increase testicle size; it merely optimises the function of existing cellular machinery. Foods rich in zinc, including oysters, red meat, and pumpkin seeds, support testicular function without physically enlarging the organs.
Vitamin D3 receptor expression in sertoli cells
Sertoli cells within the seminiferous tubules express vitamin D receptors, suggesting important roles for this nutrient in supporting spermatogenesis and testicular function. Vitamin D deficiency has been associated with reduced testosterone levels and impaired sperm quality, highlighting the nutrient’s importance in male reproductive health. Adequate vitamin D status supports optimal testicular function but cannot increase organ size . Sun exposure and dietary sources such as fatty fish provide natural vitamin D, supporting the cellular processes within existing testicular architecture.
Omega-3 fatty acids and luteinising hormone response
Omega-3 fatty acids, particularly EPA and DHA, influence cellular membrane composition and may affect hormone receptor sensitivity. Some studies suggest that omega-3 supplementation can enhance luteinising hormone response, potentially supporting testosterone production. These fatty acids also provide anti-inflammatory effects that may protect testicular tissue from oxidative damage. Fish oil, walnuts, and flaxseeds represent excellent dietary sources of omega-3 fatty acids that support testicular health without altering organ dimensions.
Antioxidants role in preventing testicular oxidative stress
Testicular tissue demonstrates high susceptibility to oxidative stress due to intensive metabolic activity and oxygen consumption during spermatogenesis. Antioxidant compounds from various foods help neutralise reactive oxygen species that could damage cellular structures and impair hormone production. Vitamins C and E, selenium, and polyphenols from fruits and vegetables provide protective effects against testicular oxidative damage. These protective mechanisms maintain optimal testicular function but do not influence physical size parameters.
The testicles operate as sophisticated biochemical factories where nutrition supports optimal function rather than structural enlargement.
Scientific literature analysis on dietary interventions
Comprehensive analysis of peer-reviewed research reveals no credible evidence supporting the claim that dietary interventions can increase testicular size. Multiple studies examining various nutritional approaches, including specific foods, supplements, and dietary patterns, consistently demonstrate that while nutrition affects testicular function and hormone production, physical enlargement remains scientifically implausible. The distinction between functional improvement and structural modification represents a crucial concept often misunderstood in popular discussions about male reproductive health.
Research examining the relationship between nutrition and testicular health typically focuses on parameters such as sperm quality, hormone levels, and cellular function rather than organ size. Studies investigating testosterone-boosting foods like pomegranates, brazil nuts, and leafy greens show potential benefits for hormonal profiles and antioxidant status. However, none of these investigations report changes in testicular volume or dimensions. The scientific consensus clearly establishes that dietary factors influence testicular performance rather than physical characteristics .
Large-scale epidemiological studies examining dietary patterns and male reproductive health provide additional insight into nutrition’s role in testicular function. Mediterranean diet adherence, characterised by high consumption of fruits, vegetables, fish, and healthy fats, correlates with better sperm parameters and hormone profiles. These population-level findings reinforce the importance of overall dietary quality for testicular health while providing no evidence for size enhancement through nutritional means.
Clinical trials investigating specific nutrients and testicular outcomes demonstrate the complexity of nutritional effects on male reproductive health. Zinc supplementation studies show improvements in testosterone levels among deficient individuals but no changes in testicular dimensions. Similarly, vitamin D supplementation research indicates hormone level improvements without structural modifications. These controlled studies provide the highest quality evidence regarding nutrition’s impact on testicular health and consistently refute claims about dietary testicle enlargement.
Debunking popular testicular enhancement food myths
Several foods have gained popularity as purported testicular enhancers, often based on cultural beliefs, anecdotal reports, or misinterpretation of scientific research. Examining these claims reveals the gap between popular misconceptions and biological reality. Understanding why these myths persist helps clarify the actual relationship between nutrition and testicular health.
Oysters frequently appear in discussions about foods that increase testicle size, primarily due to their exceptional zinc content. While zinc deficiency can impair testicular function, consuming oysters cannot physically enlarge testicles beyond their genetically determined size. The confusion arises from the legitimate benefits of zinc for testosterone production, which some interpret as evidence for structural enhancement. Oysters support optimal testicular function but cannot overcome biological limitations on organ size .
Pomegranate juice has attracted attention for its potential testosterone-boosting properties, leading to claims about testicular enlargement effects. Research indicates that pomegranate consumption may support hormonal health through antioxidant mechanisms and improved circulation. However, no studies demonstrate changes in testicular dimensions following pomegranate consumption. The antioxidant benefits represent genuine health effects that support testicular function without altering organ size.
Various nuts, particularly brazil nuts and walnuts, appear frequently in lists of foods claimed to increase testicle size. These nuts provide selenium, healthy fats, and other nutrients beneficial for male reproductive health. Selenium deficiency can impair sperm quality and testicular function, making adequate intake important for optimal reproductive health. Nevertheless, nut consumption cannot increase testicular volume beyond normal anatomical parameters established during development.
Popular food myths often contain kernels of nutritional truth but extrapolate far beyond scientific evidence when claiming structural changes.
Garlic represents another food frequently mentioned in testicular enhancement discussions, often citing its potential effects on testosterone levels and circulation. While garlic contains compounds that may support cardiovascular health and potentially influence hormone metabolism, no research demonstrates testicular enlargement effects. The circulation benefits of garlic consumption might support overall testicular health, but these effects remain functional rather than structural.
Medical conditions affecting testicular size and volume
Understanding legitimate medical conditions that influence testicular size provides important context for evaluating dietary claims. Various pathological conditions can cause testicular atrophy, enlargement, or asymmetry, requiring medical evaluation and treatment. These conditions highlight the distinction between pathological changes and normal anatomical variation, emphasising why dietary interventions cannot address structural testicular issues.
Testicular atrophy represents one of the most concerning conditions affecting testicle size, often resulting from hormonal imbalances, infections, trauma, or certain medications. Conditions such as Klinefelter syndrome, varicoceles, and hypogonadism can lead to reduced testicular volume and compromised function. Medical treatment for these conditions focuses on addressing underlying causes rather than dietary modifications . Testosterone replacement therapy may help restore function in some cases but cannot reverse significant structural atrophy through hormonal means alone.
Testicular torsion, infections, and inflammatory conditions can cause temporary or permanent changes in testicular size and shape. These acute conditions require immediate medical attention and cannot be addressed through nutritional interventions. The inflammatory response associated with these conditions may cause temporary enlargement followed by potential atrophy if not properly treated. Understanding these pathological processes emphasises the importance of medical evaluation for any concerns about testicular size or function.
Age-related changes in testicular volume represent normal physiological processes that occur gradually throughout adult life. Testosterone production typically declines after age 30, potentially accompanied by subtle changes in testicular size and consistency. These age-related modifications reflect natural hormonal changes rather than nutritional deficiencies. While maintaining good nutrition may support healthy aging processes, dietary interventions cannot reverse age-related testicular changes or restore youthful organ dimensions.
Evidence-based approaches to male reproductive health optimisation
Rather than pursuing unrealistic goals of testicular enlargement through diet, men can focus on evidence-based strategies that genuinely enhance reproductive health and testicular function. These approaches target the biological processes that influence hormone production, sperm quality, and overall reproductive capacity. Implementing comprehensive lifestyle modifications provides measurable benefits for testicular health while maintaining realistic expectations about anatomical limitations.
Maintaining optimal body weight represents one of the most important factors for testicular health, as obesity can negatively impact testosterone production and sperm quality. Excess adipose tissue increases aromatase activity, converting testosterone to estrogen and potentially affecting hormonal balance. A diet rich in whole foods, lean proteins, healthy fats, and complex carbohydrates supports healthy weight management while providing essential nutrients for testicular function. Regular physical activity complements dietary approaches by improving circulation, reducing inflammation, and supporting hormonal balance.
Sleep quality and stress management play crucial roles in maintaining optimal testicular function and hormone production. Chronic sleep deprivation can suppress testosterone production and impair sperm quality, while chronic stress elevates cortisol levels that may interfere with reproductive hormones. Prioritising 7-9 hours of quality sleep and implementing stress reduction techniques provides measurable benefits for testicular health . These lifestyle factors often have greater impact on reproductive function than specific dietary choices targeting supposed testicular enlargement.
Environmental toxin reduction represents another evidence-based approach to supporting testicular health. Exposure to endocrine-disrupting chemicals, heavy metals, and other environmental toxins can impair testicular function and hormone production. Choosing organic foods when possible, avoiding plastic food containers, and minimising exposure to household chemicals may help protect testicular health. These protective measures address genuine threats to reproductive function rather than pursuing unsubstantiated enhancement claims.
Regular medical monitoring allows for early detection and treatment of conditions that might affect testicular health and function. Annual physical examinations should include testicular examination and discussion of reproductive health concerns with healthcare providers. Men experiencing symptoms such as reduced libido, erectile dysfunction, or fertility concerns should seek professional evaluation rather than relying solely on dietary interventions. Professional medical care can identify treatable conditions and provide appropriate interventions when needed.
Temperature regulation represents a practical consideration for maintaining optimal testicular function, as excessive heat exposure can impair sperm production and potentially affect hormone synthesis. Wearing loose-fitting underwear, avoiding prolonged hot tub or sauna use, and maintaining appropriate scrotal temperature support natural testicular processes. These simple modifications complement nutritional approaches by addressing environmental factors that influence testicular health within normal anatomical parameters.