Vertigo affects millions of people worldwide, creating a debilitating sensation where the world appears to spin uncontrollably around them. Unlike simple dizziness or lightheadedness, vertigo represents a specific type of balance disorder that stems from problems within the vestibular system. As patients search for relief from this challenging condition, many wonder whether nasal irrigation techniques, particularly using a neti pot, might offer therapeutic benefits. The connection between nasal congestion, sinus pressure, and balance disturbances has prompted both healthcare professionals and patients to explore whether clearing nasal passages could alleviate vertigo symptoms. Understanding this potential relationship requires examining the complex anatomy of the inner ear, the mechanisms behind different types of vertigo, and the physiological effects of nasal irrigation on the interconnected systems that maintain our sense of balance and spatial orientation.
Understanding vestibular system dysfunction and vertigo pathophysiology
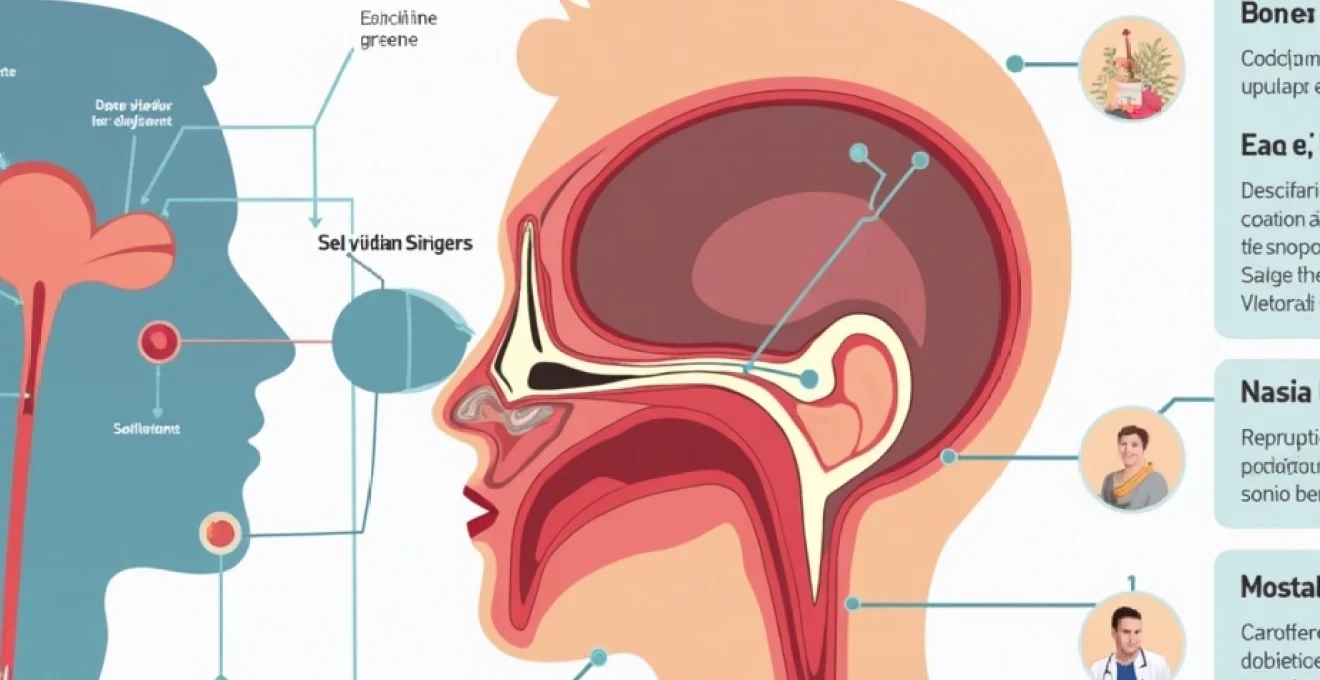
The vestibular system represents one of the most sophisticated sensory networks in the human body, comprising structures within the inner ear that detect head movements and spatial orientation. This intricate system works continuously to maintain balance and coordinate eye movements, providing essential information to the brain about our position relative to gravity and our movement through space. When dysfunction occurs within these delicate structures, the result is often vertigo—a condition that extends far beyond simple dizziness to encompass a genuine sensation of movement when no actual movement is occurring.
Inner ear anatomy: semicircular canals and otolith organs
Within each inner ear lie three semicircular canals arranged perpendicular to one another, functioning like a sophisticated three-dimensional gyroscope. These fluid-filled structures detect rotational movements in all planes of motion: horizontal, vertical forward-backward, and vertical side-to-side rotations. The canals contain specialised sensory cells called hair cells, which respond to the movement of fluid (endolymph) when the head rotates. Think of these canals as carpenter’s levels with bubbles that shift position as orientation changes.
Adjacent to the semicircular canals, the otolith organs—comprising the utricle and saccule—detect linear accelerations and the effects of gravity. These structures contain calcium carbonate crystals called otoconia, which rest upon a gelatinous membrane embedded with hair cells. When you tilt your head or experience linear movement, these crystals shift position, bending the underlying hair cells and generating neural signals that inform the brain about head position and movement.
Benign paroxysmal positional vertigo (BPPV) and otoconia displacement
BPPV represents the most common cause of peripheral vertigo, affecting approximately 2.4% of the population at some point in their lives. This condition occurs when otoconia become dislodged from their normal position within the otolith organs and migrate into one of the semicircular canals. These displaced crystals, now acting as foreign bodies within the canal, create abnormal fluid movements when the head changes position, triggering intense but brief episodes of vertigo.
The symptoms of BPPV are characteristically triggered by specific head movements, such as rolling over in bed, looking up, or bending forward. Episodes typically last less than one minute but can be accompanied by nausea and a distinctive rotatory eye movement called nystagmus. The condition doesn’t typically awaken patients from sleep, nor is it associated with hearing loss or tinnitus, distinguishing it from other vestibular disorders.
Vestibular neuritis and labyrinthitis: inflammatory vertigo triggers
Vestibular neuritis and labyrinthitis represent inflammatory conditions affecting different components of the inner ear balance system. Vestibular neuritis involves inflammation of the vestibular nerve, which carries balance information from the inner ear to the brain. This condition typically follows viral infections and causes sudden, severe vertigo that can last for days, often accompanied by nausea, vomiting, and difficulty maintaining balance.
Labyrinthitis extends beyond the nerve to involve inflammation of the entire labyrinth, including both balance and hearing structures. Patients with labyrinthitis experience vertigo symptoms similar to vestibular neuritis but also suffer from hearing loss and tinnitus. Both conditions can be triggered by upper respiratory infections, suggesting a potential connection between sinus congestion and vestibular symptoms that might respond to nasal irrigation techniques.
Ménière’s disease: endolymphatic hydrops and vertigo episodes
Ménière’s disease presents a more complex vestibular disorder characterised by episodes of vertigo lasting several hours, accompanied by fluctuating hearing loss, tinnitus, and a sensation of fullness in the affected ear. The underlying pathophysiology involves endolymphatic hydrops—an abnormal accumulation of fluid within the inner ear that increases pressure and disrupts normal vestibular and auditory function.
The episodic nature of Ménière’s disease sets it apart from other vestibular conditions, with attacks often occurring without warning and potentially awakening patients from sleep. Between episodes, patients may experience periods of relative normalcy, though progressive hearing loss typically develops over time. The fluctuating symptoms and involvement of both balance and hearing systems make this condition particularly challenging to manage.
Nasal irrigation mechanisms: saline solution effects on eustachian tube function
Nasal irrigation using devices like neti pots operates through several physiological mechanisms that could theoretically influence vestibular function. The primary action involves flushing saline solution through the nasal cavities, removing mucus, allergens, and inflammatory debris while promoting drainage of congested sinuses. This mechanical cleansing effect extends beyond simple symptom relief to address underlying inflammatory processes that might indirectly affect inner ear function through anatomical connections and shared vascular supply.
The relationship between nasal congestion and balance disturbances becomes clearer when considering the interconnected nature of the upper respiratory tract and ear structures. Chronic sinusitis and nasal inflammation can create pressure changes that affect the eustachian tubes—narrow passages connecting the middle ear to the nasopharynx. When these tubes become blocked or dysfunctional, the resulting pressure imbalances can influence inner ear fluid dynamics and potentially trigger vertigo symptoms in susceptible individuals.
Isotonic saline concentration: 0.9% sodium chloride solution preparation
The effectiveness of nasal irrigation depends significantly on using an appropriate saline concentration that matches the body’s natural fluid composition. Isotonic saline solutions, containing 0.9% sodium chloride, provide optimal therapeutic benefits without causing irritation or cellular damage to nasal tissues. This concentration mimics the salt content of human tears and blood plasma, ensuring comfortable application while maintaining the solution’s cleansing and anti-inflammatory properties.
Proper preparation involves dissolving one teaspoon of pure salt in one pint (500ml) of distilled or previously boiled water, creating a solution that effectively thins mucus secretions without causing tissue swelling or discomfort. The temperature should be lukewarm to match body temperature, as solutions that are too hot or cold can trigger additional vestibular symptoms or cause tissue damage. Using distilled or sterile water is crucial to prevent introducing harmful microorganisms into the nasal passages.
Eustachian tube drainage: mucus clearance and pressure equalisation
Eustachian tube dysfunction represents a common link between upper respiratory congestion and balance problems. These tubes normally open and close regularly during swallowing, yawning, and other activities to equalise pressure between the middle ear and atmospheric pressure. When inflammation from sinus infections or allergic reactions causes tissue swelling, the eustachian tubes may become blocked, creating pressure differentials that can influence inner ear function.
Nasal irrigation helps restore eustachian tube function by reducing inflammation in the nasopharyngeal region where these tubes terminate. By clearing mucus and reducing tissue swelling, saline irrigation can improve tube patency and restore normal pressure equalisation mechanisms. This effect may be particularly beneficial for individuals whose vertigo symptoms are related to pressure changes or underlying sinus pathology.
Middle ear ventilation: tympanic membrane mobility enhancement
The middle ear requires adequate ventilation to maintain proper function of the tympanic membrane and the delicate chain of bones (ossicles) that transmit sound vibrations. When eustachian tube dysfunction occurs, negative pressure can develop within the middle ear space, reducing tympanic membrane mobility and potentially affecting the transmission of pressure waves to the inner ear. These pressure changes might influence vestibular function, particularly in individuals with pre-existing inner ear conditions.
Effective nasal irrigation can help restore middle ear ventilation by addressing the underlying inflammatory conditions that compromise eustachian tube function. As nasal congestion decreases and inflammation subsides, the tubes can resume their normal opening and closing patterns, allowing proper pressure equalisation and potentially alleviating vertigo symptoms that are secondary to middle ear dysfunction.
Nasopharyngeal decongestion: reducing adenoid tissue inflammation
The nasopharynx contains adenoid tissue that can become enlarged and inflamed, particularly in response to chronic infections or allergic reactions. Enlarged adenoids can mechanically obstruct eustachian tube openings, contributing to pressure problems that affect both hearing and balance. Additionally, chronic inflammation in this region can spread to adjacent structures, potentially influencing vestibular function through vascular or neural pathways.
Regular nasal irrigation with saline solutions can help reduce adenoid inflammation by removing irritants and inflammatory mediators from the nasopharyngeal region. This anti-inflammatory effect may indirectly benefit vestibular function by improving overall upper respiratory health and reducing the chronic inflammation that can affect interconnected structures throughout the head and neck region.
Clinical evidence: neti pot efficacy for vestibular disorders
Current scientific evidence regarding neti pot effectiveness for vertigo treatment remains limited, with most research focusing on nasal irrigation benefits for sinusitis and allergic rhinitis rather than vestibular disorders specifically. However, several clinical observations and case reports suggest potential benefits for certain types of vertigo, particularly when symptoms are associated with upper respiratory congestion or chronic sinusitis. The lack of randomised controlled trials specifically examining nasal irrigation for vertigo reflects the complexity of vestibular disorders and the challenge of isolating nasal irrigation effects from other therapeutic interventions.
Studies investigating nasal irrigation for sinus-related symptoms have demonstrated consistent benefits including reduced inflammation, improved mucus clearance, and decreased medication requirements for chronic sinusitis patients. These findings suggest that individuals whose vertigo symptoms are secondary to sinus pathology or eustachian tube dysfunction might experience improvements through regular nasal irrigation. The challenge lies in identifying which vertigo patients are most likely to benefit from this intervention , as the underlying causes of vestibular symptoms vary significantly between individuals.
Clinical experience from otolaryngologists treating patients with concurrent sinus disease and vestibular symptoms indicates that addressing upper respiratory inflammation can sometimes lead to improvements in balance symptoms. However, these observations require careful interpretation, as vertigo symptoms can fluctuate naturally, and patients often receive multiple concurrent treatments that make it difficult to isolate the specific effects of nasal irrigation. More rigorous research is needed to establish clear evidence-based recommendations for neti pot use in vertigo management.
The interconnected nature of upper respiratory and vestibular systems suggests that comprehensive treatment approaches addressing both nasal congestion and balance symptoms may provide superior outcomes compared to treating these conditions in isolation.
Contraindications and risk assessment for nasal irrigation in vertigo patients
While nasal irrigation is generally considered safe for most individuals, certain contraindications and risk factors require careful consideration, particularly in patients with vertigo who may already have compromised balance or underlying medical conditions. Patients with active ear infections, perforated tympanic membranes, or recent ear surgery should avoid nasal irrigation until these conditions resolve, as forcing saline solution through connected passages could worsen existing problems or introduce infections into sterile spaces.
Individuals with severe nasal obstruction from polyps, deviated septum, or other structural abnormalities may experience difficulty with nasal irrigation and could potentially force contaminated material into the eustachian tubes if proper technique is not followed. The risk becomes particularly concerning for immunocompromised patients or those with chronic medical conditions that affect wound healing or infection resistance. Proper assessment by a healthcare provider can help identify patients who might benefit from nasal irrigation versus those who should avoid this intervention .
The use of contaminated water represents one of the most serious risks associated with nasal irrigation, as rare but potentially fatal infections with organisms like Naegleria fowleri have been reported. Always use distilled, sterile, or previously boiled water for nasal irrigation solutions, and maintain strict hygiene protocols for cleaning and storing irrigation devices. Replace neti pots and other irrigation equipment regularly to prevent bacterial colonisation that could lead to secondary infections.
Patients experiencing severe vertigo should exercise particular caution when performing nasal irrigation, as the head positioning required for effective irrigation might trigger additional balance symptoms or increase fall risk. Consider performing irrigation while seated or with assistance until symptoms stabilise. Additionally, some individuals may experience temporary worsening of congestion or drainage following irrigation, which could theoretically affect eustachian tube function and influence vestibular symptoms in the short term.
Alternative vestibular rehabilitation techniques: epley manoeuvre and canalith repositioning
While nasal irrigation may provide supportive benefits for certain types of vertigo, evidence-based vestibular rehabilitation techniques offer more direct and proven interventions for specific vestibular disorders. The Epley manoeuvre represents the gold standard treatment for BPPV affecting the posterior semicircular canal, with success rates exceeding 80% when performed correctly. This technique uses specific head and body movements to relocate displaced otoconia from the semicircular canal back to their appropriate position within the otolith organs.
The Epley manoeuvre involves a series of precise head rotations and body position changes performed in a specific sequence over several minutes. Patients begin sitting upright, then move through various positions including lying back with the head extended and rotated, followed by side-lying positions before returning to upright. Each position is held for approximately 30 seconds to allow gravity to guide the displaced crystals through the canal system. The technique requires proper instruction from trained healthcare providers to ensure safe and effective execution .
Alternative canalith repositioning procedures include the Semont manoeuvre, which uses rapid position changes to achieve crystal relocation, and the Brandt-Daroff exercises, which can be performed at home to help maintain treatment benefits. These techniques specifically address the mechanical displacement of otoconia that causes BPPV, offering direct treatment of the underlying pathophysiology rather than symptomatic relief. Success rates vary depending on the specific canal involved and the skill of the practitioner performing the manoeuvre.
Vestibular rehabilitation therapy extends beyond canalith repositioning to include balance retraining exercises, gaze stabilisation techniques, and habituation protocols designed to reduce motion sensitivity. These comprehensive programmes address the adaptive changes that occur in the central nervous system following vestibular injuries, helping patients develop compensation strategies and improve overall balance function. Modern vestibular rehabilitation incorporates virtual reality technology, dynamic platform training, and customised exercise protocols tailored to individual patient needs and functional goals.
For patients with Ménière’s disease, treatment approaches focus on dietary modifications including salt restriction, diuretic medications, and in severe cases, surgical interventions such as endolymphatic sac decompression or vestibular ablation procedures. These treatments address the underlying fluid imbalances and pressure changes that characterise this condition, offering more targeted therapeutic approaches than general supportive measures like nasal irrigation.
Integration of multiple treatment modalities often provides optimal outcomes for complex vestibular disorders. Patients may benefit from combining canalith repositioning procedures with vestibular rehabilitation exercises, medication management, and supportive interventions such as dietary modifications or stress management techniques. The key to successful treatment lies in accurate diagnosis of the underlying vestibular condition and selection of appropriate evidence-based interventions rather than relying solely on symptomatic treatments that may provide temporary relief without addressing root causes.