The prevailing misconception that hemorrhoids exclusively affect older adults has led many young people to overlook early symptoms or dismiss the possibility of developing this common condition. Hemorrhoids, medically known as piles , represent swollen veins in the anal and rectal area that can affect individuals across all age groups, including teenagers and young adults. Recent clinical data indicates that approximately 15-20% of hemorrhoid cases occur in people under 30, challenging the traditional belief that this condition predominantly impacts the elderly population.
Understanding hemorrhoid development in younger demographics requires examining the unique physiological and lifestyle factors that contribute to increased intra-abdominal pressure and compromised anal cushion integrity. The modern lifestyle patterns of prolonged sitting, dietary modifications, and stress-related bowel dysfunction create a perfect storm for hemorrhoid development in adolescents and young adults. This comprehensive analysis explores the pathophysiology, risk factors, diagnostic approaches, and evidence-based treatment strategies specifically relevant to hemorrhoid management in younger patient populations.
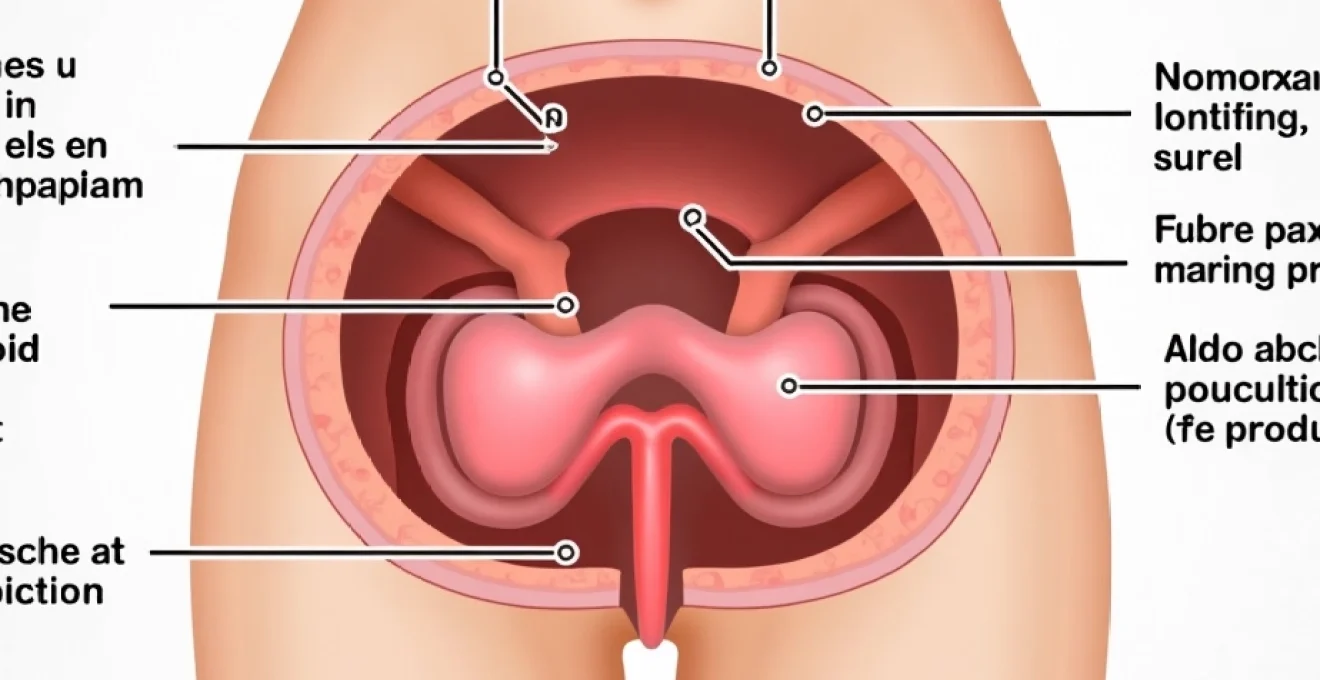
Haemorrhoid pathophysiology in adolescents and young adults
Vascular cushion development during puberty
The anal vascular cushions undergo significant developmental changes during puberty, making adolescents particularly susceptible to hemorrhoidal complications. These highly vascularised tissue structures, composed of arteriovenous communications, smooth muscle fibres, and elastic connective tissue, experience rapid growth spurts that can compromise their structural integrity. During adolescence, hormonal fluctuations affect collagen synthesis and vascular wall elasticity, potentially predisposing young individuals to early hemorrhoid formation. The increased blood flow associated with pubertal development places additional strain on these delicate vascular structures.
Hormonal fluctuations and anal cushion integrity
Hormonal changes during puberty significantly impact the integrity of anal cushions through multiple mechanisms. Oestrogen and progesterone fluctuations affect venous compliance and smooth muscle tone within the anal canal, whilst growth hormone surges influence connective tissue maturation patterns. These hormonal variations can lead to weakened supporting structures and increased venous distensibility, creating conditions favourable for hemorrhoid development. Young women may experience particular vulnerability during menstrual cycles when hormonal fluctuations are most pronounced, affecting both vascular tone and bowel movement patterns.
Connective tissue maturation in the anorectum
The anorectal region undergoes extensive connective tissue remodelling during adolescence and early adulthood. The Parks’ ligament and Treitz’s muscle fibres, which provide crucial support to the anal cushions, may not achieve full maturation until the mid-twenties. This delayed maturation process leaves young people with inadequately supported vascular structures that are more prone to prolapse and engorgement. Genetic variations in collagen synthesis can further compromise tissue strength, explaining why some young individuals develop hemorrhoids despite minimal risk factor exposure.
Increased intra-abdominal pressure during growth spurts
Rapid growth during adolescence creates unique biomechanical challenges that can precipitate hemorrhoid formation. The disproportionate growth of the torso relative to pelvic structures can alter intra-abdominal pressure dynamics, particularly during Valsalva manoeuvres. Athletic young adults engaging in resistance training or competitive sports may experience repeated episodes of elevated intra-abdominal pressure that stress the anal vascular cushions. Weight training activities commonly performed by teenagers and young adults can generate pressures exceeding 200 mmHg, significantly straining the delicate hemorrhoidal vessels.
Clinical risk factors specific to the 16-25 age demographics
Sedentary lifestyle and prolonged sitting behaviours
The modern educational and professional environment exposes young people to unprecedented levels of prolonged sitting, creating ideal conditions for hemorrhoid development. University students spend an average of 8-10 hours daily in seated positions, combining lecture attendance, study sessions, and recreational screen time. This prolonged sitting reduces venous return from the anal region whilst increasing pressure on the hemorrhoidal cushions. Gaming culture and social media consumption further exacerbate this problem, with many young adults spending additional hours in sedentary positions outside of academic or work commitments.
The physiological impact of prolonged sitting extends beyond simple mechanical pressure. Extended periods of immobility reduce overall circulation, leading to venous stasis and increased susceptibility to thrombosis formation within hemorrhoidal vessels. The popularity of bean bags, low-sitting furniture, and floor-based seating arrangements among young people may worsen these effects by promoting sustained flexion of the hip joints and compression of pelvic vessels.
Dietary patterns and Low-Fibre consumption habits
Contemporary dietary patterns among young people create significant challenges for maintaining healthy bowel function and preventing hemorrhoid formation. The prevalence of processed foods, fast food consumption, and irregular meal patterns contributes to chronic constipation and straining during defecation. University students and young professionals often rely on convenience foods that are typically low in fibre and high in refined carbohydrates, creating hard, difficult-to-pass stools that require excessive straining.
Energy drink consumption and excessive caffeine intake among young adults can further complicate bowel patterns by causing dehydration and altering normal gastrointestinal motility. The combination of inadequate hydration, irregular eating schedules, and poor food choices creates a perfect storm for constipation-related hemorrhoid development. Social dining patterns, including frequent alcohol consumption and late-night eating, disrupt normal circadian rhythms that regulate bowel function.
University Stress-Related constipation and straining
Academic pressure and lifestyle transitions associated with university attendance create unique stressors that significantly impact bowel function in young adults. The gut-brain axis responds to psychological stress by altering intestinal motility, often resulting in constipation-predominant bowel dysfunction. Examination periods, assignment deadlines, and social pressures can trigger stress responses that inhibit normal defecation reflexes, leading to prolonged stool retention and subsequent straining during bowel movements.
Sleep deprivation, commonly experienced by university students, further compounds these effects by disrupting the normal circadian regulation of bowel function. All-night study sessions and irregular sleep patterns can severely impact the natural morning gastrocolic reflex, forcing young people to strain during bowel movements at suboptimal times. The combination of stress-induced constipation and time pressure often leads to hurried, forceful attempts at defecation that can traumatise hemorrhoidal tissues.
Athletic activities and heavy lifting complications
Young athletes and fitness enthusiasts face unique risks for hemorrhoid development due to the nature of their training activities. Weightlifting, powerlifting, and resistance training require repeated Valsalva manoeuvres that dramatically increase intra-abdominal pressure. These pressure spikes can reach levels of 300-400 mmHg during maximal lifts, placing enormous strain on the anal vascular cushions. The popularity of CrossFit, strongman training, and functional fitness movements among young adults has increased exposure to these risk factors.
Endurance sports participation can also contribute to hemorrhoid development through different mechanisms. Long-distance cycling, rowing, and equestrian activities involve prolonged pressure on the perineal region, potentially compromising circulation to the anal area. Dehydration associated with intense training can lead to constipation, whilst the use of sports supplements and protein powders may alter normal bowel patterns in susceptible individuals.
Pregnancy-related haemorrhoids in young women
Young women experiencing pregnancy face dramatically increased risks for hemorrhoid development due to multiple physiological changes occurring simultaneously. The growing uterus places direct pressure on pelvic vessels, compromising venous return from the anal region. Hormonal changes during pregnancy, particularly increased progesterone levels, cause smooth muscle relaxation and venous dilatation that predisposes to hemorrhoid formation. Morning sickness and dietary restrictions during early pregnancy can lead to constipation, further increasing the risk of straining-related hemorrhoid development.
The physiological demands of labour and delivery create additional challenges for young women. The prolonged Valsalva efforts required during the second stage of labour can cause acute hemorrhoid prolapse and thrombosis. Postpartum constipation, often related to pain medication use and fear of bowel movements, can perpetuate hemorrhoidal problems in the weeks following delivery.
Diagnostic challenges in paediatric and young adult proctology
Symptom presentation variations in younger patients
Young patients often present with atypical hemorrhoid symptoms that can complicate accurate diagnosis and delay appropriate treatment. Unlike older adults who typically report classic symptoms of bleeding and prolapse, young people may primarily complain of anal discomfort, itching, or a sensation of incomplete evacuation. Social embarrassment and reluctance to discuss anal symptoms can lead to delayed presentation, allowing conditions to progress to more severe stages before medical attention is sought.
The psychological impact of hemorrhoid symptoms may be particularly pronounced in younger patients who may lack understanding of the condition’s commonality and treatability. Anxiety about the implications of rectal bleeding or anal pain can lead to catastrophic thinking and avoidance behaviours that further delay diagnosis. Young patients may also attribute symptoms to other causes, such as dietary indiscretions or temporary stress-related bowel changes, leading to inappropriate self-treatment attempts.
Digital rectal examination considerations for adolescents
Performing digital rectal examinations in adolescent and young adult patients requires special consideration of psychological comfort, consent issues, and anatomical variations. Privacy concerns and body image sensitivity are often heightened in this age group, necessitating careful explanation of the examination process and its necessity for accurate diagnosis. The presence of a chaperone becomes particularly important when examining young patients, and same-gender healthcare providers may be preferred when possible.
Technical considerations for digital rectal examination in young patients include the typically smaller anal aperture and potentially increased anal sphincter tone due to anxiety or embarrassment. Adequate lubrication and gentle technique become even more critical to ensure patient comfort and cooperation. The examination may reveal different findings compared to older patients, with less tissue laxity and more prominent muscular contractions that can obscure palpable abnormalities.
Anoscopy and proctoscopy protocols for young adults
Anoscopic examination in young adults requires modified protocols to ensure optimal visualisation whilst maintaining patient comfort and cooperation. The standard adult anoscope may be too large for some younger patients, necessitating the use of paediatric or adolescent-sized instruments. Pre-procedure counselling becomes crucial to explain the importance of the examination and address any misconceptions about discomfort or invasiveness.
The anoscopic findings in young hemorrhoid patients often differ from those seen in older populations. Internal hemorrhoids may appear less prominent due to better tissue elasticity, whilst external components may be more reactive and inflamed. The examination technique may need modification to account for increased sphincter tone and patient anxiety, potentially requiring topical anaesthetics or anxiolytic premedication in some cases.
Differential diagnosis including anal fissures and perianal abscesses
Young patients presenting with anorectal symptoms require careful differentiation between hemorrhoids and other common conditions affecting this age group. Anal fissures are particularly common in young adults and can present with similar symptoms of pain and bleeding. The sharp, tearing pain characteristic of fissures typically occurs during and immediately after bowel movements, contrasting with the duller, more persistent discomfort associated with hemorrhoids. Chronic constipation patterns common in young people can predispose to both conditions simultaneously, complicating the clinical picture.
The distinction between hemorrhoids and other anorectal conditions in young patients often requires multiple assessment modalities and careful symptom analysis to ensure accurate diagnosis and appropriate treatment selection.
Perianal abscesses represent another important differential diagnosis in young patients, particularly those with risk factors such as compromised immune function or inflammatory bowel disease. The acute onset of severe pain, fever, and localised swelling helps distinguish abscesses from hemorrhoidal conditions. However, thrombosed external hemorrhoids can occasionally mimic the presentation of small perianal abscesses, requiring careful clinical judgement and sometimes diagnostic aspiration to confirm the diagnosis.
Evidence-based treatment approaches for young haemorrhoid patients
Treatment strategies for hemorrhoids in young patients must balance immediate symptom relief with long-term prevention of recurrence, considering the patient’s life expectancy and future risk factors. Conservative management approaches are typically favoured initially, given the better healing capacity and tissue resilience characteristic of younger patients. Dietary modification and lifestyle interventions often produce more dramatic improvements in young people compared to older adults, making these interventions the cornerstone of initial treatment approaches.
Pharmacological interventions in young patients require consideration of age-appropriate formulations and potential long-term effects. Topical treatments containing local anaesthetics, anti-inflammatory agents, and astringent compounds can provide effective symptom relief whilst supporting natural healing processes. The use of oral medications, including fibre supplements, stool softeners, and anti-inflammatory agents, should be tailored to the patient’s specific symptoms and underlying risk factors.
Minimally invasive procedures such as rubber band ligation, sclerotherapy, and infrared coagulation are increasingly being utilised in young patients with persistent symptoms despite conservative management. These procedures offer excellent outcomes in younger populations due to superior healing capacity and typically require shorter recovery periods. The psychological impact of invasive procedures may be more pronounced in young patients, necessitating comprehensive pre-procedural counselling and post-procedural support.
Surgical interventions, including hemorrhoidectomy and stapled hemorrhoidopexy, are reserved for severe cases that fail to respond to conservative and minimally invasive approaches. Young patients typically experience better surgical outcomes with lower complication rates and faster recovery times compared to older adults. However, the decision to pursue surgical treatment must carefully weigh the immediate benefits against the potential for long-term complications and the impact on quality of life during critical life stages such as university attendance or early career development.
Preventive strategies and lifestyle modifications for youth
Effective hemorrhoid prevention in young people requires comprehensive lifestyle modifications that address the unique risk factors prevalent in this demographic. Educational initiatives targeting young adults should emphasise the importance of regular physical activity, proper sitting posture, and frequent position changes during prolonged sedentary activities. University health services and workplace wellness programmes play crucial roles in implementing these preventive strategies on a population level.
Dietary interventions must be practical and sustainable for young adults with busy lifestyles and limited cooking skills. Emphasising easily accessible high-fibre foods, adequate hydration strategies, and meal planning techniques can help young people maintain healthy bowel function despite challenging schedules. The integration of fibre-rich snacks, portable fruit and vegetable options, and convenient hydration reminders can significantly impact bowel health outcomes.
Prevention strategies must be tailored to the unique lifestyle challenges faced by young adults, including irregular schedules, limited resources, and competing priorities that may impact adherence to recommended interventions.
Stress management techniques specifically designed for young adults can address the psychological factors contributing to bowel dysfunction and hemorrhoid development. Mindfulness practices, time management strategies, and healthy coping mechanisms can help mitigate the impact of academic and professional stressors on gastrointestinal function. Sleep hygiene education and regular exercise programmes support both stress reduction and healthy bowel patterns, creating synergistic effects for hemorrhoid prevention.
Technology-based interventions, including mobile applications for hydration tracking, fibre intake monitoring, and posture reminders, can leverage young people’s comfort with digital platforms to support preventive behaviours. Gamification of healthy behaviours and peer support networks through social media platforms can enhance motivation and adherence to preventive strategies among young adults.
Long-term prognosis and recurrence prevention in Early-Onset cases
Young patients diagnosed with hemorrhoids typically experience excellent long-term outcomes when appropriate treatment and prevention strategies are implemented early in the disease course. The superior healing capacity and tissue resilience characteristic of younger individuals often result in complete symptom resolution with conservative management approaches. However, the extended life expectancy of young patients makes long-term recurrence prevention particularly important, as lifestyle factors and anatomical changes over decades can significantly impact future hemorrhoid risk.
Early intervention and education programmes have been shown to reduce recurrence rates significantly in young adults with hemorrhoid histories. Patients who receive comprehensive education about risk factors, preventive strategies, and early symptom recognition demonstrate better long-term outcomes compared to those receiving only acute treatment. The establishment of healthy bowel habits during young adulthood can have profound impacts on gastrointestinal health throughout the lifespan.
The development of structured follow-up protocols for young hemorrhoid patients can help identify and address recurrence risk factors before symptoms become problematic. Regular monitoring of bowel habits, lifestyle changes, and symptom patterns allows healthcare providers to intervene early when preventive measures may be most effective. Annual or biannual check-ups during the young adult years can provide opportunities to reinforce education, assess compliance with preventive strategies, and identify new risk factors that may have emerged due to life changes such as career transitions, pregnancy, or altered activity levels.
Genetic predisposition factors in young patients with hemorrhoid histories warrant special consideration for long-term management strategies. Individuals with family histories of hemorrhoidal disease or connective tissue disorders may require more aggressive preventive approaches and closer monitoring throughout their adult years. The identification of these high-risk patients early in their clinical course allows for implementation of targeted interventions that can significantly reduce the likelihood of severe recurrent disease. Personalised risk assessment tools incorporating both genetic and lifestyle factors can help guide long-term management decisions and resource allocation for young hemorrhoid patients.
Life stage transitions present unique challenges for young adults with hemorrhoid histories, requiring adaptive management strategies that accommodate changing circumstances. Career establishment, relationship formation, pregnancy planning, and residential changes can all impact the effectiveness of previously successful preventive strategies. Healthcare providers must work collaboratively with young patients to anticipate these transitions and develop flexible management plans that can evolve with changing life circumstances while maintaining effective hemorrhoid prevention.
The investment in comprehensive hemorrhoid management during young adulthood yields significant dividends in terms of quality of life preservation and healthcare cost reduction over the patient’s entire lifespan.
Research outcomes indicate that young adults who actively participate in structured hemorrhoid prevention programmes demonstrate recurrence rates of less than 15% over ten-year follow-up periods, compared to 35-40% recurrence rates in patients receiving only acute treatment. These data underscore the importance of comprehensive, patient-centred approaches to hemorrhoid management in younger populations. The economic implications of effective early intervention extend beyond immediate healthcare costs to include reduced workplace absenteeism, improved productivity, and enhanced quality of life metrics that justify initial investment in comprehensive care approaches. Long-term studies continue to demonstrate that the most successful outcomes occur when young patients become active partners in their own care, developing the knowledge and skills necessary to maintain optimal anorectal health throughout their adult years.