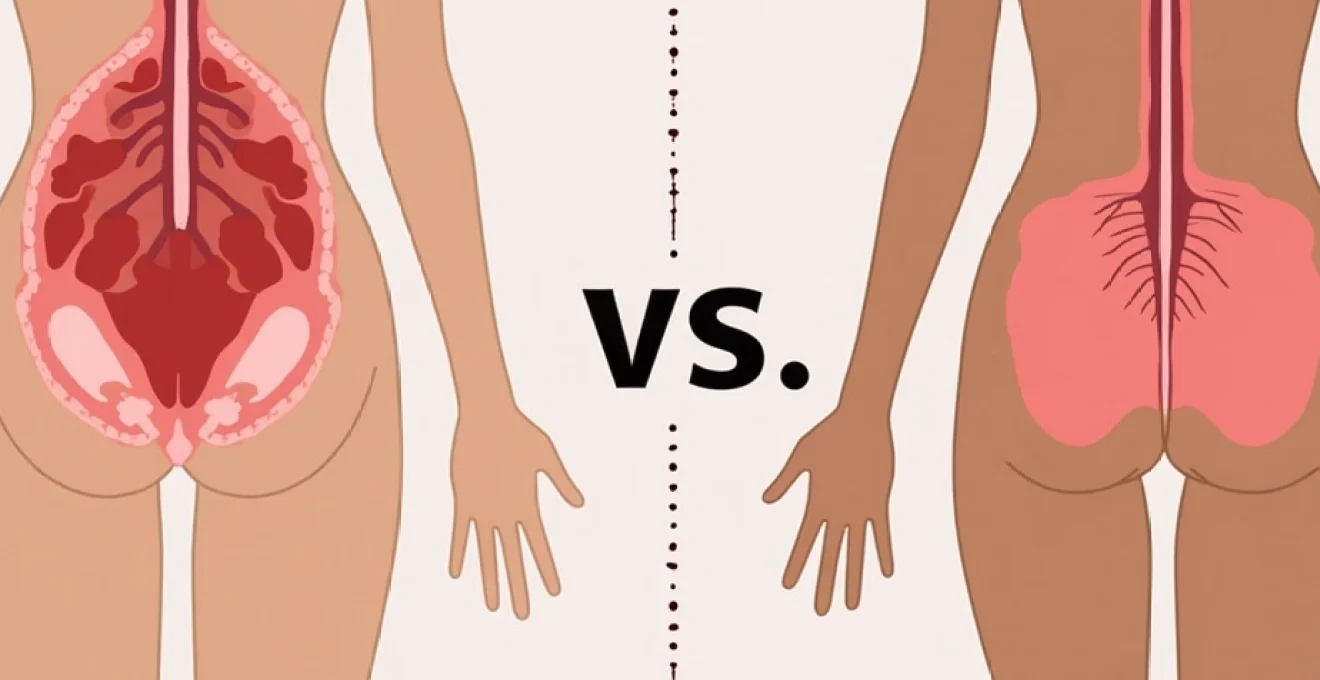
The experience of pain during medical abortion and spontaneous labour represents one of the most significant concerns for individuals facing these procedures. Recent research has revealed that many people undergoing medical abortion report pain levels that exceed their initial expectations, with some comparing the intensity to labour contractions. Understanding the physiological mechanisms, pain characteristics, and management strategies for both experiences enables healthcare providers to offer more comprehensive counselling and support. The complexity of pain perception in these contexts involves multiple factors including prostaglandin activity, uterine contractions, individual pain tolerance, and psychological preparedness.
Medical abortion, achieved through mifepristone followed by misoprostol administration, triggers a cascade of physiological responses that closely mirror certain aspects of natural labour. However, the pain patterns, duration, and intensity differ significantly between these two experiences. Current evidence suggests that while medical abortion pain may be more intense than many anticipate, it typically follows different temporal patterns compared to spontaneous labour contractions.
Pharmacological pain mechanisms in medical abortion using mifepristone and misoprostol
The two-drug protocol for medical abortion initiates pain through distinct pharmacological pathways that create uterine contractions and cervical changes. Mifepristone, a selective progesterone receptor modulator, blocks the hormone essential for pregnancy maintenance while increasing prostaglandin sensitivity. This initial medication primes the uterus for the subsequent misoprostol administration, though it rarely causes significant pain on its own.
Misoprostol, a synthetic prostaglandin E1 analogue, triggers the primary pain-generating mechanisms in medical abortion. When administered 24-48 hours after mifepristone, it binds to prostaglandin receptors in uterine smooth muscle, initiating powerful contractions designed to expel pregnancy tissue. These contractions generate pain through several mechanisms: direct mechanical stimulation of pain receptors, ischemia from intense muscle contractions, and inflammatory mediator release.
Prostaglandin E1 analogue effects on myometrial contractions
Misoprostol’s action on myometrial tissue creates contractions that differ qualitatively from natural labour patterns. The prostaglandin E1 receptor activation causes immediate calcium release within smooth muscle cells, leading to sustained, often irregular contractions. Unlike the gradual buildup typical of early labour, these pharmacologically-induced contractions can reach significant intensity within hours of administration. Research indicates that prostaglandin-mediated contractions tend to be less coordinated than oxytocin-driven labour contractions, potentially contributing to the unpredictable pain patterns many individuals experience.
Cervical ripening and dilatation pain pathways
The cervical changes induced by misoprostol contribute substantially to the overall pain experience during medical abortion. Prostaglandin E1 breaks down cervical collagen fibres and increases tissue compliance, allowing for rapid dilatation. This process activates nociceptors in cervical tissue, creating sharp, cramping sensations that many describe as distinct from menstrual pain. The speed of cervical change, often occurring over hours rather than the gradual progression seen in labour, can intensify the associated discomfort significantly.
Cramping intensity progression through gestational stages
Pain intensity during medical abortion correlates directly with gestational age, as larger pregnancy tissue requires stronger uterine contractions for expulsion. Studies demonstrate that individuals undergoing medical abortion at 8-9 weeks gestation report higher maximum pain scores compared to those at earlier stages. The uterine muscle must generate greater contractile force to expel more developed tissue, leading to more intense and prolonged cramping episodes. This relationship explains why pain duration also increases with advancing gestational age.
Anti-inflammatory response and endorphin release patterns
The body’s natural pain-modulating systems respond differently during pharmacologically-induced abortion compared to spontaneous labour. While both processes trigger endorphin release, the rapid onset of medical abortion pain may overwhelm natural analgesic mechanisms. The inflammatory cascade initiated by prostaglandins can actually sensitise pain pathways, making subsequent contractions feel more intense. This phenomenon, known as peripheral sensitisation, may explain why some individuals find medical abortion pain more difficult to tolerate than anticipated.
Physiological pain characteristics during spontaneous labour contractions
Natural labour pain follows predictable physiological patterns that have evolved to facilitate safe delivery while providing neurological feedback about progress. The pain serves multiple biological functions: signalling labour onset, encouraging position changes that aid delivery, and preparing the body for the intense physical demands of childbirth. Understanding these mechanisms helps explain why labour pain, despite potentially lasting many hours, may feel more manageable to some individuals than the concentrated intensity of medical abortion.
Labour contractions are orchestrated by complex hormonal interactions involving oxytocin, prostaglandins, and other signalling molecules. This natural progression allows for gradual pain escalation, giving the body time to adapt and deploy coping mechanisms. The predictable pattern of contraction and rest periods provides psychological relief and physical recovery time between pain episodes.
Three-stage labour pain progression and neural transmission
Labour pain follows a characteristic three-phase progression that reflects the underlying physiological changes occurring during delivery. Early labour typically involves mild, irregular contractions that gradually increase in strength and frequency. The pain pathways involved include both visceral afferents from the uterus and cervix, transmitted through sympathetic nerve fibres to the spinal cord at T10-L1 levels. During this phase, many individuals can continue normal activities between contractions, as the pain intensity remains moderate and manageable.
Visceral pain receptors in uterine muscle fibres
The uterine muscle contains specialised pain receptors that respond to mechanical stretch, ischemia, and chemical mediators released during contractions. These nociceptors become increasingly sensitive as labour progresses, partly due to the release of substance P and other pain-enhancing molecules. The density and sensitivity of these receptors vary among individuals, contributing to the wide range of labour pain experiences reported. Unlike the pharmacologically-triggered pain of medical abortion, natural labour allows for gradual receptor sensitisation, potentially making the pain more tolerable despite longer duration.
Referred pain patterns in lower back and pelvic region
Labour pain commonly manifests as referred sensations in the lower back, pelvis, and upper thighs due to the shared neural pathways between the uterus and these regions. This pain distribution pattern, known as dermatomal referral, occurs because visceral pain fibres converge with somatic nerve fibres at the spinal cord level. Approximately 30% of labouring individuals experience significant back pain, particularly when the fetal head positions against the sacrum. This referred pain component is less common in medical abortion, where pain typically remains localised to the lower abdomen.
Oxytocin-induced contraction strength and pain correlation
Natural oxytocin release during labour creates a positive feedback loop that intensifies contractions progressively while simultaneously triggering endogenous opioid release. This physiological design helps manage increasing pain levels as labour advances. Oxytocin receptors in the uterus become more numerous and sensitive as pregnancy progresses, allowing for increasingly powerful contractions while the body’s pain-modulating systems adapt accordingly. This natural escalation differs significantly from the rapid-onset, high-intensity pain often experienced with misoprostol administration.
Comparative pain intensity assessment using validated measurement scales
Research utilising standardised pain assessment tools reveals significant differences in how individuals experience and rate pain during medical abortion versus labour. Studies employing visual analogue scales consistently show that medical abortion pain reaches higher peak intensities than many anticipate, with over 40% of participants rating their maximum pain between 8-10 on a 10-point scale. This finding challenges the common counselling practice of comparing medical abortion pain to “heavy menstrual cramps,” a comparison that proves inadequate for many individuals’ actual experiences.
Labour pain assessment presents unique challenges due to its extended duration and variable progression patterns. While peak labour pain intensities may equal or exceed those reported during medical abortion, the gradual buildup and intermittent nature of labour contractions can make the overall experience more psychologically manageable. Studies suggest that the predictability of labour pain progression, with clear rest periods between contractions, contributes to better coping mechanisms compared to the sometimes unpredictable patterns of medical abortion pain.
The subjective nature of pain reporting introduces additional complexity when comparing these experiences. Individual factors such as previous childbirth experience, cultural background, anxiety levels, and pain catastrophising tendencies significantly influence pain scores. Research indicates that nulliparous individuals often report higher pain scores for both medical abortion and labour, though their comparative assessments vary considerably based on which experience they encounter first.
Recent survey data from over 1,500 medical abortion patients revealed that nearly half experienced pain levels exceeding their expectations, with many describing the intensity as comparable to labour contractions rather than menstrual cramps.
Duration and temporal pain pattern differences between both procedures
The temporal characteristics of pain represent one of the most significant differences between medical abortion and spontaneous labour. Medical abortion pain typically concentrates into a relatively brief but intense period, usually lasting 2-6 hours from misoprostol administration to tissue expulsion. This compressed timeframe can make the experience feel overwhelming, as individuals must cope with significant pain intensity without the extended adjustment period characteristic of natural labour.
Labour pain follows a more protracted pattern, often developing over 12-20 hours for first-time mothers and 6-12 hours for multiparous individuals. This extended timeline allows for gradual psychological and physiological adaptation to increasing pain levels. The predictable pattern of contractions followed by pain-free intervals provides crucial recovery time and helps maintain psychological resilience throughout the process.
The unpredictability of medical abortion pain patterns adds another layer of complexity to the experience. While some individuals experience steady cramping that builds to a crescendo before tissue expulsion, others report intermittent waves of intense pain interspersed with relatively comfortable periods. This variability makes it challenging to prepare individuals mentally for what they might experience, contrasting with labour where the general progression pattern is more consistent.
Pain trajectory patterns identified in qualitative research include four distinct types: minimal overall discomfort, brief intense episodes, intermittent cramping waves, and sustained high-level pain. Understanding these patterns helps healthcare providers offer more tailored counselling and pain management strategies. The inability to predict which pattern an individual will experience represents a significant difference from labour, where pain progression follows more predictable stages.
Pharmaceutical pain management protocols for medical abortion versus labour
Pain management approaches for medical abortion and labour require different pharmaceutical strategies due to their distinct mechanisms and timing constraints. Medical abortion pain management focuses on prophylactic and immediate relief measures that can be safely administered in outpatient settings, while labour pain management encompasses a broader range of options including regional anaesthesia techniques available in hospital environments.
Current evidence supports the use of non-steroidal anti-inflammatory drugs as first-line therapy for medical abortion pain, with ibuprofen showing superior efficacy compared to paracetamol alone. The prostaglandin-mediated nature of medical abortion pain makes NSAIDs particularly effective, as they directly inhibit the cyclooxygenase enzymes responsible for prostaglandin synthesis. Timing of administration proves crucial, with prophylactic dosing often more effective than reactive treatment.
Nsaids efficacy: ibuprofen and diclofenac comparative analysis
Ibuprofen remains the gold standard NSAID for medical abortion pain management, with studies demonstrating optimal efficacy at 400-600mg doses administered prophylactically with misoprostol. The drug’s dual mechanism of action—reducing prostaglandin synthesis while providing direct anti-inflammatory effects—makes it particularly suitable for this indication. Diclofenac offers comparable efficacy but requires more careful dosing considerations due to its potency and potential gastrointestinal effects. Both medications show superior performance when administered before pain onset rather than as rescue therapy.
Opioid analgesia considerations: codeine and tramadol applications
Opioid medications serve as second-line options for medical abortion pain management, reserved for individuals with contraindications to NSAIDs or those requiring additional analgesia. Tramadol, with its dual mechanism involving opioid receptor activation and monoamine reuptake inhibition, shows promise for severe medical abortion pain. However, its potential for nausea and dizziness can compound the side effects already associated with misoprostol. Codeine combinations provide moderate efficacy but carry risks of respiratory depression and dependency, requiring careful patient selection and monitoring.
Regional anaesthesia options: epidural versus paracervical block
Regional anaesthesia techniques remain largely unavailable for outpatient medical abortion due to logistical and safety constraints, contrasting sharply with labour where epidural anaesthesia provides highly effective pain relief. Paracervical blocks, while technically feasible, are rarely employed for medical abortion due to the procedure’s ambulatory nature and the need for sterile conditions. This limitation represents a significant difference in pain management options between the two experiences, with labour patients having access to more comprehensive anaesthetic interventions.
Complementary pain relief: TENS units and heat therapy effectiveness
Non-pharmacological pain relief methods play important supportive roles in both medical abortion and labour pain management. Transcutaneous electrical nerve stimulation units provide variable efficacy, with some individuals reporting significant relief while others find minimal benefit. Heat therapy, including heating pads and warm baths, offers accessible relief options that can be safely combined with pharmacological approaches. The effectiveness of these methods often depends on individual preferences and the specific pain patterns experienced, making them valuable adjunctive options rather than standalone solutions.
Individual pain tolerance variables and predicting factors
Individual pain tolerance represents a complex interaction of physiological, psychological, and social factors that significantly influence the experience of both medical abortion and labour pain. Genetic variations in pain receptor sensitivity, previous pain experiences, anxiety levels, and cultural attitudes toward pain all contribute to the wide range of reported pain intensities. Understanding these variables helps healthcare providers offer more personalised counselling and pain management strategies tailored to individual risk factors and preferences.
Age and parity status emerge as consistent predictors of pain intensity in both contexts, with younger, nulliparous individuals typically reporting higher pain scores. However, previous childbirth experience can influence pain perception in complex ways—while some individuals find medical abortion pain more manageable based on their labour experience, others report the opposite. The compressed timeframe and different pain characteristics of medical abortion can make direct comparisons challenging even for those with extensive labour experience.
Psychological factors, particularly anxiety and pain catastrophising tendencies, significantly impact pain perception during both medical abortion and labour. Research demonstrates that individuals with higher baseline anxiety scores report more intense pain experiences and require more comprehensive pain management interventions. The element of choice and control also influences pain perception, with planned procedures often better tolerated than emergency situations. This psychological component explains why comprehensive pre-procedure counselling can substantially improve pain management outcomes.
Cultural and social support factors play crucial roles in pain perception and coping mechanisms. Individuals with strong support systems report better pain tolerance and more positive overall experiences during both medical abortion and labour. Cultural attitudes toward pain expression and management can influence help-seeking behaviours and treatment preferences. Healthcare providers must consider these individual variables when developing pain management plans and setting realistic expectations for both medical abortion and labour experiences.
| Pain Characteristic | Medical Abortion | Spontaneous Labour |
|---|---|---|
| Peak Intensity | 8-10/10 (40% of cases) | 7-9/10 (variable) |
| Duration | 2-6 hours | 6-20 hours |
| Pattern | Variable/unpredictable | Progressive waves |
| Location | Lower abdomen | Abdomen/back/pelvis |
The relationship between gestational age and pain intensity requires special consideration in medical abortion counselling. As pregnancy advances, the uterine contractions required for tissue expulsion become stronger and more prolonged, leading to increased pain levels. This correlation helps predict individual pain experiences and guide appropriate analgesic selection. Individuals undergoing procedures at later gestational ages should receive enhanced pain management protocols and more intensive monitoring during the recovery period.
Pain management expectations must account for individual variations while providing realistic information about typical experiences. The challenge lies in preparing individuals adequately without creating unnecessary anxiety or fear. Evidence suggests that detailed, honest counselling about pain possibilities, combined with comprehensive management strategies, leads to better patient satisfaction and fewer complications compared to minimising pain discussions or providing
incomplete counselling about unrealistic pain expectations.
The evidence consistently shows that individuals who receive comprehensive pain counselling, including realistic discussions about potential intensity and duration, report higher satisfaction rates and better pain management outcomes. This approach requires healthcare providers to balance honesty about pain realities with reassurance about available management strategies. Effective counselling should include discussion of the four identified pain trajectory patterns, allowing individuals to understand the range of possible experiences while developing personalised coping strategies.
Predicting individual pain responses remains challenging despite identified risk factors. While age, parity, gestational age, and anxiety levels provide useful guidance, significant individual variation persists within these categories. Healthcare providers should use these predictive factors as starting points for pain management planning rather than definitive indicators. The development of validated pain prediction tools specific to medical abortion could significantly improve patient counselling and resource allocation in the future.
Support system availability emerges as a crucial but often overlooked factor in pain management success. Research demonstrates that individuals with dedicated support persons report lower pain scores and require fewer interventions during both medical abortion and labour. This finding highlights the importance of encouraging patients to arrange appropriate support and providing guidance on how support persons can most effectively assist during the pain experience.
Healthcare providers must individualise pain management approaches based on patient-specific risk factors, previous experiences, and cultural considerations while maintaining realistic expectations about both medical abortion and labour pain intensities.
The integration of individual pain tolerance assessment into routine clinical practice requires systematic approaches that go beyond simple pain history taking. Validated screening tools for anxiety, pain catastrophising, and previous trauma experiences can help identify patients requiring enhanced pain management protocols. However, these assessments must be conducted sensitively, avoiding stigmatisation while ensuring appropriate resource allocation for those at highest risk for severe pain experiences.
Training healthcare providers to recognise and address individual pain tolerance variables represents an essential component of quality reproductive healthcare. This training should encompass not only pharmacological knowledge but also communication skills for discussing pain expectations and cultural competency for working with diverse patient populations. The goal remains providing compassionate, evidence-based care that acknowledges individual differences while maintaining realistic expectations about both medical abortion and labour pain experiences.